
Electronic health records (EHRs) have made life easier for patients and healthcare professionals. However, concerns about EHR security have also been raised. Strong security measures for EHRs not only maintain patient satisfaction and loyalty but also ensures that your organization complies with laws governing patient medical records. Discover effective strategies for safeguarding patient information with these helpful tips.
An electronic health record (EHR) usually contains various types of information such as contact details, details of visits to healthcare providers, allergies, insurance details, family medical history, immunization status, information on existing health conditions, medications list, records of hospital stays, and details of any surgeries or procedures conducted.
Governments globally are striving to ensure that all citizens receive standardized electronic health records with uniform information. Cost remains a significant barrier to the adoption of electronic health records.
Electronic health record (EHR) standards are in place to verify that electronic health records meet meaningful use requirements, ensuring they have the necessary technical abilities and security measures in place. Standards also aim to improve interoperability within the health IT community. Notable standards for interoperability include:
Health Level Seven International (HL7), which establishes global criteria for exchanging clinical and administrative data.
Fast Healthcare Interoperability Resources (FHIR), a web-based toolkit that operates under HL7.
SMART Health IT, is an open technology platform that supports the development of applications capable of functioning across different healthcare systems, including EHRs.
Electronic health records are now commonly used to store and share patient information, but this online storage method can also make patients vulnerable to privacy breaches and theft.
This type of personal data is highly valuable on the black market. Even lower-level criminals can cause significant harm to patients’ credit and identity through such breaches.
Naturally, healthcare data breaches can greatly harm patients. Identity theft, fraudulent credit card openings, and unauthorized purchases of medications are all potential consequences. Patients may also be vulnerable to scam phone calls that appear genuine due to leaked personal details.
A data breach is a serious issue. In 2021 alone, more than 40 million patient records were compromised. The largest breach impacted over 3 million individuals, and these are just the cases reported to the federal government. Some incidents likely remain undetected and unreported.
The mishandling of data does not only impact patients but also harms healthcare providers. Breaches in electronic health records (EHRs) can result in various consequences such as:
Additionally, healthcare providers may suffer reputation damage and financial loss, and even face the risk of financial collapse.
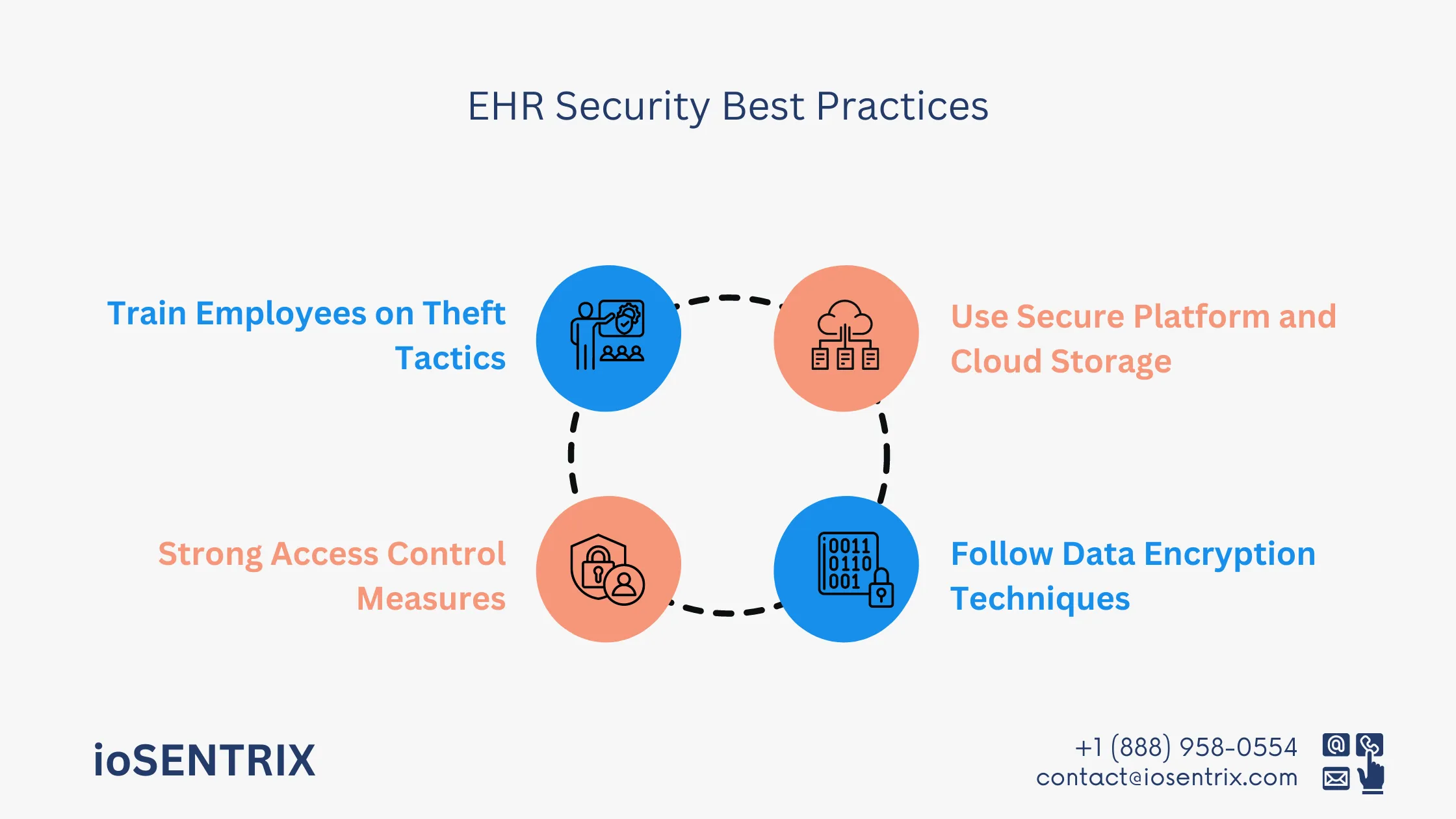
Below are security techniques for EHR that medical practice can implement to minimize unauthorized access to EHRs and protect against data breaches.
It is crucial to select electronic health record (EHR) management systems that are known for their safety and dependability. You can determine the reputation of these systems by reading reviews from other practices and conducting online research to check for any reported security breaches.
Similarly, it is crucial to ensure the security of any cloud storage systems you utilize. In many cases, cloud storage is interconnected with EHR platforms. However, if you also rely on on-site storage servers, it is advisable to follow these steps:
When transferring patient data between healthcare providers, such as from a general physician to a surgeon, the information is vulnerable. Even though it may not be mandatory by law, encryption is highly recommended for safeguarding patient records and ensuring both providers and patients have peace of mind.
It is important to use encryption while sending medical records, referrals, test results, and prescriptions. Different institutions and locations may have varying encryption standards. When transmitting information across state lines, you may need to employ higher encryption standards. Healthcare providers should also follow non-U.S. regulations when sharing records internationally, especially for patients traveling or residing outside the United States.
Everyone doesn’t need to have access to patient files. Limit the individuals handling patient EHRs to reduce the risk of breaches. Using designated digital devices for accessing patient data is another way to control access. Tablets carried by providers between rooms are a more secure option than having a computer in each exam room. If desktop computers are inevitable, make sure that employees log off promptly after use and consider adding an automatic log-off feature for extra security.
It is not recommended to allow the use of personal devices to access medical records due to security risks. In the past, healthcare providers used to bring paper charts home for documentation or log in to records from personal computers when they were digitized. Although there may be scenarios where providers need to access records remotely, it is advisable to provide them with a secure work laptop equipped with encryption for such purposes.
All new employees should undergo training on data security procedures, with annual refresher sessions to stay updated on new regulations and security measures. Employees should be careful not to leave computer screens open when not in use, especially in busy areas like the emergency room where it is tempting to leave windows open for quick access.
Staff should be informed about current phishing scams and other email schemes used to steal patient information. If they are unsure about the legitimacy of an email or any other communication, they should consult a clinic supervisor or IT professional for verification.
As per the Morsani College of USF Health, the performance of a computer in sharing and receiving healthcare data is influenced by its age and location, particularly in urban or rural settings. Setting up an EHR system may pose challenges in rural areas compared to urban regions due to connectivity issues. Therefore, it’s important to choose a location for your practice that facilitates easy EHR implementation. If faced with poor connectivity, consider upgrading your plan or switching to a more reliable internet provider for seamless operations.
An essential goal of incorporating EHRs is to enhance the efficiency of your staff’s tasks. However, improper customization of EHR systems may disrupt your existing workflow. To avoid this challenge, ensure that the EHR provider you select showcases how the integration aligns with the unique requirements of your pediatric practice.
As stated by USF Health, healthcare providers and patients may have worries about privacy issues when using EHRs. Common concerns involve potential data loss from events like natural disasters or cyberattacks. It is crucial to understand the privacy measures and procedures in place in your new EHR system before its implementation to address these concerns properly.
The team at ioSENTRIX is here to help with all your EHR system needs. Whether you want to implement, switch, or upgrade your current system, our consultants, developers, and trainers are ready to assist you. Our best services help you get the most out of your NextGen EHR system. With our top tips and tricks, we ensure your success both now and in the future.
We provide valuable advice to help you optimize your practice. Through practical training, you and your team can effectively manage your electronic health record systems. To discover how ioSENTRIX can enhance your pediatric practice, feel free to contact us today.